GPs in England will receive a £20 bonus each time they avoid directly referring a patient to a hospital, as part of a new scheme aimed at reducing NHS waiting lists. The initiative, which has a total funding of up to £80 million, is designed to reduce the number of unnecessary hospital appointments by encouraging GPs to first consult specialists via phone or online before making a referral. This process, known as ‘Advice and Guidance’ (A&G), aims to ensure that patients receive appropriate care in the most efficient manner possible.
Under the A&G scheme, GPs will determine whether a patient needs a hospital referral or if alternative treatment options could be explored first. These alternatives may include prescribing medication, sending patients for preliminary scans or blood tests, or directing them to community services like physiotherapy. Between July and December 2024, around 660,000 treatments were diverted from hospitals into the community via this process, although uptake has been inconsistent across the country.
The Department of Health and Social Care hopes that by offering financial incentives, the scheme will increase the number of treatments diverted from hospitals to community care, with a goal of reaching 2 million diversions by the end of 2025/26. The department estimates that half of all A&G consultations will result in a referral to the hospital, while the remainder will be advised to pursue alternative care options. GP practices will receive the £20 payment for utilizing the A&G service, regardless of the final outcome, and decisions on routine matters are typically returned within a week.
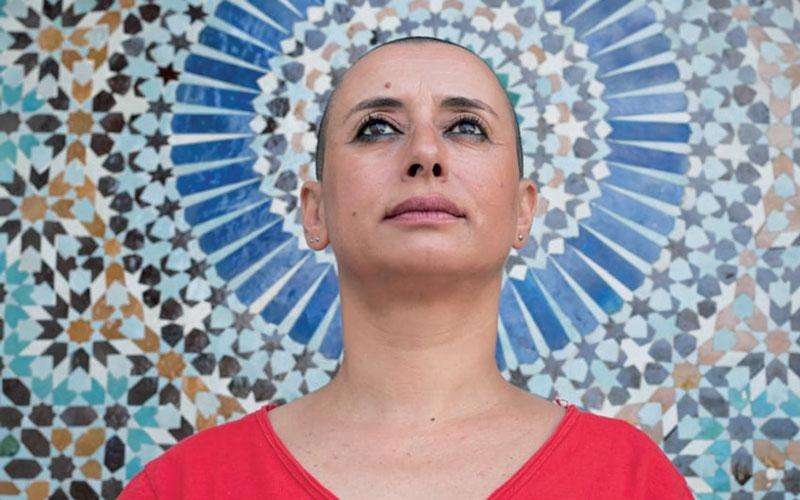
Health Minister Karin Smyth expressed that the initiative would help provide care closer to home, saving patients time and reducing the number of unnecessary hospital visits. She said, "By caring for patients closer to home, we save time and stop masses of people having to head to the hospital for unnecessary appointments in the first place. We are rewiring the NHS to do things differently, more efficiently, and deliver better outcomes for patients."
However, the scheme has attracted concerns from patient advocacy groups. Some warn that the focus on reducing referrals could risk delaying essential care, particularly for patients who genuinely need hospital treatment. Beccy Baird from The King’s Fund, a health think tank, emphasized that effective implementation of the scheme is critical. She noted that financial incentives for GPs based on the number of A&G consultations could potentially undermine the primary goal of delivering high-quality care. Baird called for safeguards to ensure that the scheme does not introduce unnecessary hurdles for patients seeking treatment.
Dennis Reed, director of Silver Voices, a campaign group for elderly patients, expressed skepticism about the scheme’s ability to meet its ambitious goals. He warned that community services are already stretched due to high demand, and there may not be enough resources to handle the increase in patients being redirected away from hospitals. Reed raised concerns that vulnerable patients, particularly the elderly, could miss out on vital care, as had occurred in previous community healthcare reforms, such as those involving mental health care.
The Department of Health and Social Care suggested that the A&G scheme could benefit certain patient groups, including those with menopausal symptoms, irritable bowel syndrome, or ear, nose, and throat issues, as these conditions may be managed without the need for hospital treatment. Ruth Rankine, director of primary care at the NHS Confederation, highlighted that if implemented effectively, the scheme could support improved patient care, streamline the referral process, and make more efficient use of NHS resources. Rankine stressed that for many conditions, hospital treatment is not always the best option.
The British Medical Association (BMA), which had previously called on GPs to boycott the A&G service as part of industrial action, has since negotiated the scheme with the government. Dr. Katie Bramall-Stainer, chair of the BMA’s GP committee for England, welcomed the new initiative, acknowledging it as a small but necessary step in addressing the long-standing issue of underinvestment in general practice. She said the scheme would help GPs provide better care for patients in the community, while also supporting practices with additional funding.
The NHS is currently facing a backlog of 6.24 million people on waiting lists, with some waiting more than 18 months for treatment. Health Secretary Wes Streeting has pledged to reduce the number of patients waiting for more than 18 weeks to 92% by the end of the current Parliament. Despite the concerns surrounding the A&G scheme, the government hopes that the combination of financial incentives and innovative solutions will help ease pressure on the NHS and improve patient care across the country.






.svg)




