Doctor who has been warned that doctors "don't stand a chance" if they voice concerns was asked for his fingerprints by NHS authorities who are looking for a whistleblower.
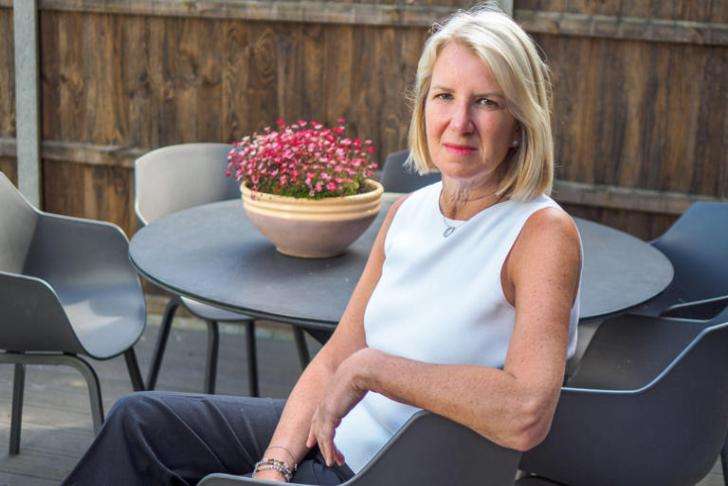
Anaesthesiologist and critical care specialist Patricia Mills declared she would "never be the same again" after being harassed by supervisors who also insisted on getting samples of her handwriting.
They were attempting to determine who wrote a letter to a widower with allegations on a member of staff that provided care for his late wife, who passed away in 2018 at Bury St. Edmunds' West Suffolk Hospital.
The hospital's "incendiary" and unusual request for staff fingerprints was the subject of a report ordered by NHS England. Later on, the hospital's CEO resigned due to what was perceived as a "witch hunt."
Physicians have accused NHS management of persecuting them for speaking out, and they now want the government to establish a new criminal offense of causing harm to whistleblowers.
This comes as additional leakers charged that the NHS was "defending" managers who had come under fire for how they handled patient safety alerts. In the health service, several have been assigned to other senior positions.
More than fifty clinicians have expressed worries to The Telegraph that they were singled out after raising the alarm over up to 170 patient fatalities and nearly 700 patient injuries; one specialist has called the actual number of preventable deaths "astronomical."
Whistleblowers claim that rather of attempting to address issues that could be endangering patients, NHS executives are allegedly using millions of taxpayer dollars to hire private investigators and law companies to look into these issues.
Bosses at West Suffolk Hospital sought to fingerprint a number of employees, including Dr. Mills, following the anonymous letter that was delivered to Jon Warby, whose wife, Susan, passed away following surgery for a perforated colon.
The letter claimed that an anesthetist who performed Mrs. Warby's surgery had "injected himself with drugs...while in charge of a patient and it was all hushed up," alleging that the hospital had covered it up. The letter's writer has never been identified.
Those who refused to hand over fingerprints claim they were told by the trust that “refusal to provide consent or refusal to provide an adequate rationale could be considered as evidence that the individual was involved in writing the letter.”
Dr. Mills informed The Telegraph that she became ill as a result of the West Suffolk NHS Trust's action because she was afraid for her job. She refused to be fingerprinted or provide a handwriting sample.
Whistleblowers, she claimed, "absolutely don't stand a chance" against the authority of NHS managers, who frequently invested large sums of public funds in looking into the whistleblowers' personal lives.
Dr Mills told The Telegraph: “I was off work at the time for six months. I’ve never, ever had any time off work, ever. It made me very unwell.
“I will never be the same again,” she said, adding that: “But it wasn’t just me. It had a profound effect on everyone who was persecuted, really, by their employer. I wasn’t the only one, there were several others.”
Dr. Mills requested assistance from the National Guardian's Office, an organization established to make sure health and care providers follow whistleblower laws, in contesting the trust's request for her fingerprints. She deemed their response to be "literally useless."
A report into the matter commissioned by NHS England later stated: “The requests for fingerprints were incendiary. No evidence was produced to me that fingerprinting had previously been used in the NHS in a potential disciplinary investigation such as this, where the police had already confirmed that there was no evidence that a criminal act had been committed.”
It said the trust’s pursuit of the whistleblower had lacked “fairness, balance and compassion” and was “disproportionate and inappropriate.”
When the search for the whistleblower became public in 2020, the trust's then-CEO, Steve Dunn, resigned. Dr. Mills is still employed with the trust.
Dr. Mills thinks that because of the exceptional outcome of her case—senior executives losing their jobs—she was able to go back to work.
The NHS manager assessment process has to be changed, according to the whistleblower.
She said: “I think there’s a very good case for a ‘fit and proper persons’ test deciding that if you have persecuted someone who has raised patient safety concerns, then there’s no place for you in the NHS.”
The anesthetist mentioned in the letter was not personally accountable for Mrs. Warby's death, according to the results of an inquest into her death.
Dr Ewen Cameron, chief executive of West Suffolk NHS Foundation Trust, said: “We accept full responsibility and have apologised to the staff and family affected by the failings surrounding the whistleblowing case…
“Whilst we’ve come a long way, we know there is more to do.”
On Thursday, at the Royal Society of Medicine in London, Justice for Doctors, a group for whistleblowers that was established during the epidemic and has been holding regular online meetings ever since, conducted its first patient safety conference in person.
The founder of the organization, Salam Al-Sam, explained to the audience that the NHS's treatment of whistleblowers was a result of a "fear culture," which discouraged many employees from coming forward.
_2.jpg)
_1.jpg)





.svg)


